In modern dentistry, dental implant technology has become one of the preferred solutions for restoring missing teeth. While many people may have a basic understanding of the implant procedure, the term healing abutment often remains unfamiliar.
In fact, it plays a crucial behind-the-scenes role in the dental restoration process—serving as a bridge between the implanted fixture in the jawbone and the final restoration (such as a dental crown).
But what exactly is a healing abutment? How does it function during the healing phase of dental implantation?
What scientific principles lie behind its material, shape, and functional design?
This article will unveil the mystery of the healing abutment and explore its essential role in successful dental implant rehabilitation.
Healing abutment for dental implant
The healing abutment, also known as a touca de cura ou gingiva former, plays a vital role in the dental implant restoration process by promoting the healing of both soft and hard tissues around the implant. This precision-engineered component not only supports healthy gingival recovery, but also acts as a protective barrier for the implant site—preventing the accumulation of plaque and food debris and thereby maintaining cleanliness and health in the surgical area.
Typically, the healing abutment is carefully attached to the top of the dental implant. It is designed with a slightly larger diameter than the implant itself. This thoughtful design enhances the abutment’s stability and serves a key function during the healing phase—helping to shape the ideal gingival contour and providing an esthetic foundation for the final prosthetic restoration.
During the implant procedure, oral surgeons may place the healing abutment during either a one-stage or two-stage surgery, depending on the individual case. Regardless of the approach, the healing abutment remains an indispensable component for successful implant restoration, quietly supporting the harmonious integration between the implant and surrounding tissues.
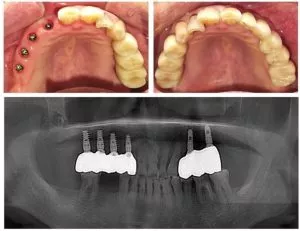
Instalação do pilar de cicatrização
During dental implant treatment, the method of installing the healing abutment varies depending on the surgical approach—primarily categorized as either a one-stage or two-stage procedure.
In a one-stage surgery, the oral surgeon places both the implant and the healing abutment (also referred to as a healing cap) in a single operation. First, the implant is precisely inserted into the pre-planned position in the alveolar bone. Then, the healing abutment is securely attached on top of the implant. At this point, the healing abutment protrudes above the gumline and remains in place throughout the healing period. This exposed design helps guide the soft tissue to heal in an ideal contour. Over time, osseointegration occurs—where the implant fuses firmly with the surrounding jawbone. Once this fusion is complete, the healing abutment is removed to expose the implant, allowing the placement of a final abutment, which will support the dental crown. The custom-made crown is then precisely attached, completing the implant restoration process.
In contrast, a two-stage surgery begins with the implant being placed into the jawbone, after which the site is covered with gum tissue and left to heal. Over the course of several months, the implant slowly integrates with the surrounding bone through osseointegration. In the second stage, the surgeon reopens the gum to expose the implant and attaches the healing abutment. During this stage, the healing abutment continues to guide gingival healing and shape the soft tissue architecture in preparation for the final restoration.
One key reason some patients and clinicians opt for the use of a healing abutment—especially in a one-stage approach—is the potential to shorten the overall treatment time. Once the healing abutment is placed, there is typically no need for a second surgery to uncover the implant. After soft tissue healing, the healing abutment can simply be replaced with the final abutment, followed by the crown installation. This reduces the number of surgical interventions, minimizes patient discomfort and inconvenience, and shortens the treatment duration—allowing patients to regain normal chewing function and aesthetic appearance more quickly.
Nonetheless, whether a one-stage or two-stage approach is chosen, the decision depends on a comprehensive assessment of each patient’s specific conditions, including bone quality, gum health, and general health status. The goal is always to ensure the highest success rate and long-term stability of the dental implant restoration.
Os pilares de cicatrização não devem ser reutilizados
In dental implant treatments, healing abutments (also known as healing caps) play a vital role in promoting the healing of tissues around the implant and guiding the gingival contour. However, healing abutments are classified as single-use medical consumables and should not be reused. There are several rigorous and critical reasons behind this guideline.
From a surface characteristics perspective, even after thorough sterilization, the original surface condition of a new healing abutment cannot be fully restored. During manufacturing, healing abutments undergo special surface treatments that create a specific microstructure and chemical composition designed to support cell attachment, proliferation, and differentiation. This facilitates optimal healing of the surrounding soft and hard tissues. However, reprocessing through sterilization—especially using high-temperature autoclaving or chemical disinfectants—can irreversibly alter the titanium surface’s original properties and microstructure. These changes may reduce the biocompatibility of the abutment, diminish its effectiveness in promoting tissue healing, and potentially trigger localized inflammation, thereby affecting the overall success of the implant.
Cleaning is another major reason healing abutments are unsuitable for reuse. In order to remove residual tissue, blood, and bacterial contamination, a thorough cleaning is required. However, the cleaning process itself carries inherent risks. The screw portion of the healing abutment is finely engineered, often with complex threads that are difficult to clean completely without causing damage. Using hard brushes, high-pressure rinsing, or improper cleaning agents can lead to deformation, abrasion, or even breakage of the threads. Once compromised, the abutment may not be securely fastened to the implant, leading to loosening or detachment during normal oral functions such as chewing or speaking. This instability can disrupt tissue healing and may lead to peri-implantitis or other complications, jeopardizing the long-term stability of the dental implant.
From an infection control standpoint, reusing healing abutments increases the risk of cross-contamination. While modern sterilization technologies are highly effective, they cannot guarantee 100% eradication of all pathogens. Resistant bacteria, viruses, or unique infectious agents may survive the sterilization process. If a contaminated healing abutment is reused on another patient, it could lead to serious medical safety issues and pose unnecessary health risks.
To ensure the safety and effectiveness of dental implant treatments and to protect both oral and overall patient health, healing abutments must be used strictly in accordance with single-use protocols. This is not only a matter of patient safety but also a fundamental requirement of medical standards and ethical responsibility. During the implant process, clinicians must carefully manage the quality and usage of medical components to provide patients with high-quality, reliable care.

What is the difference between healing abutment and final abutment?
There are clear differences between a pilar de cicatrização and a pilar definitivo (also known as a permanent abutment) in terms of timing of use, function, and appearance. Below is a detailed explanation:
Timing of Use
- Pilar de cicatrização: Installed immediately after the dental implant surgery. At this stage, the implant has just been placed into the alveolar bone, and the healing abutment is used to shape and stabilize the surrounding gum and soft tissues. It helps guide proper gingival formation, creating ideal conditions for the later prosthetic phase.
- Pilar definitivo: Placed after complete healing and osseointegration of the implant with the surrounding bone tissue. This process typically takes several months. Once the implant is securely fused with the jawbone, the final abutment is connected to support the prosthetic crown.
Função
- Pilar de cicatrização: Its main role is to support and shape the surrounding soft tissues during healing. It guides the gum to grow in the correct form, helping to create a healthy gingival cuff. This helps prevent food debris and bacteria from entering the area around the implant, reducing the risk of infection.
- Pilar definitivo: Provides structural support for the dental crown, enabling the patient to chew and speak normally. It securely connects the crown to the implant and transmits the chewing forces, ensuring the long-term functionality and stability of the implant.
Appearance
- Pilar de cicatrização: Has a relatively simple appearance and is not designed for aesthetics. Its primary goal is functional—ensuring proper soft tissue healing and stability.
- Pilar definitivo: Aesthetics are crucial. It must blend seamlessly with surrounding teeth and gums to achieve a natural look. Its color, shape, and surface finish are customized based on the patient’s oral anatomy and cosmetic requirements to make the final restoration look as natural as possible.
Vantagens da utilização de um pilar de cicatrização
1. Promotes Healthy Tissue Healing
Guides Gingival Shaping:
A healing abutment acts like a “mold,” guiding the gum tissue to grow in an ideal shape. During dental implantation, it’s crucial for the gum to form a proper cuff to surround the implant and abutment, preventing food debris and bacteria from entering and thus lowering the risk of infection. With its specific shape and size, the healing abutment provides direction for gingival growth, allowing the tissue to closely adapt around the implant and form a healthy gingival cuff.
For anterior implants, where aesthetics are especially important, the healing abutment helps shape a natural and symmetrical gum contour, making the implant visually harmonious with adjacent teeth.
Maintains Soft Tissue Space:
After implant placement, the surrounding soft tissue may shrink or shift. The healing abutment occupies space to prevent excessive tissue shrinkage and preserve enough soft tissue volume for the future crown. It’s similar to building a house: a frame must be set first to ensure structural space. Without a healing abutment, the gum may recede, resulting in gaps between the gum and crown that not only affect appearance but also increase the risk of food impaction and periodontal disease.
2. Increases Implant Success Rate
Promotes Osseointegration:
Healing abutments help stabilize the implant within the alveolar bone and minimize micro-movement. Osseointegration—the integration of bone with the implant—is vital for implant success, and even slight movement can disrupt the attachment and growth of bone cells. By securely connecting to the implant, the healing abutment offers solid support, encouraging bone cells to adhere and grow along the implant surface. This accelerates osseointegration and improves overall success rates.
Reduces Risk of Infection:
During the healing phase, the healing abutment serves as a barrier that protects the implant from oral bacteria and debris—acting like a “defensive line.” Its smooth surface makes it easier to clean, allowing patients to maintain oral hygiene around the implant site, further reducing the likelihood of infection. Infections during this phase can lead to peri-implantitis or even implant failure, so using a healing abutment helps effectively prevent these complications.
3. Optimizes Prosthetic Outcomes
Facilitates Crown Fabrication:
The healing abutment plays a crucial role in positioning and supporting the future crown. It serves as an accurate reference for crown design and fabrication. Dentists can use the location and contour of the healing abutment to design a crown that fits tightly with the implant and maintains proper occlusion. This is similar to tailoring clothes—using a suitable mannequin (healing abutment), the tailor can cut and sew garments (crown) that fit perfectly.
Achieves Aesthetic Restoration:
In highly visible areas like the front teeth, the healing abutment helps shape ideal gingival form and height, ensuring that the final crown matches the surrounding natural teeth in appearance. It mimics the natural gingival contour, making the implant tooth look more lifelike and satisfying patients’ aesthetic expectations. For patients with gum recession caused by missing teeth, the healing abutment can guide gingival regrowth, resulting in full and naturally shaped gums that blend seamlessly with the final restoration.
4. Shortens Treatment Time (in Certain Cases)
Advantage of One-Stage Surgery:
In one-stage implant procedures, the healing abutment is placed at the same time as the implant. This allows the healing process to begin immediately, eliminating the need for a second surgery—as in two-stage procedures—after the implant has fused with the bone. As a result, the overall treatment duration is significantly reduced, enabling faster implant restoration and return to normal life. This is a major benefit for patients eager to resolve tooth loss efficiently.
Comparison Between Implant Healing Abutment and Cover Screw
In dental implant procedures, the implant healing abutment and cover screw serve different purposes. They differ significantly in function, timing of use, appearance, and placement:
Função
- Parafuso de cobertura: Primarily used to temporarily seal the implant and protect it from external tissue interference. It aids in ensuring a sterile environment around the implant, promoting smooth osseointegration (bone integration). It enhances the initial stability of the implant and prevents bacterial contamination during the healing phase.
- Pilar de cicatrização: Connects the implant with the future prosthetic restoration. It guides the growth of gingival tissue, reshapes the soft tissue, forms a proper gingival cuff, and creates space for the final restoration. It facilitates tissue healing around the implant.
Timing of Use
- Parafuso de cobertura: Usually placed immediately after implant insertion and removed once the surrounding tissue has fully healed.
- Pilar de cicatrização: Generally placed several weeks or months after implant placement, depending on implant stability and the patient’s oral health. It remains in place until the final restoration is completed.
Appearance
- Parafuso de cobertura: Typically a visible metal screw placed at the top of the implant.
- Pilar de cicatrização: Usually made of plastic or metal and placed onto the implant but is not visible in the mouth.
Placement
- Parafuso de cobertura: Installed on the top of the implant to seal the internal cavity and prevent external contaminants from entering.
- Pilar de cicatrização: Placed on the implant to support gingival tissue growth and prepare for crown placement.
FAQ
1. How long does a healing abutment last?
A healing abutment can typically last over 10 years. With proper care, it may last 20, 40 years, or even a lifetime. However, the actual duration varies from person to person and depends on factors such as the material of the healing abutment and post-surgery oral care.
2. Is a healing abutment necessary?
Yes, a healing abutment is generally essential in dental implant procedures. After the implant is placed, the healing abutment provides a stable foundation for the new artificial root, allowing the surrounding bone and soft tissues to heal and integrate properly. It helps shape the gum and supports tissue recovery. Without it, the gum may not heal well, increasing the risk of infection and potentially reducing the long-term success of the implant.
3. Can you chew on a healing abutment?
Chewing is not recommended in the early stage after a healing abutment is placed. The gum tissue needs time to adapt and heal. Chewing too soon can cause the abutment to loosen or shift, compromising implant stability. Within the first 1–2 weeks, avoid biting, especially on hard, sticky, or hot foods. Stick to soft, easy-to-digest foods like porridge, noodles, and eggs, and maintain good oral hygiene. Between 2–4 weeks, you may gradually try softer foods like bread and fruit, but control your bite force. After 4 weeks, if healing progresses well without pain or swelling, you can slowly return to a normal diet—just avoid very hard items like nuts and bones.
4. Why do healing abutments fall out?
Healing abutments can fall out due to several reasons:
- Poor oral hygiene during healing: Can lead to infection and inflammation around the abutment, causing loosening.
- Chewing hard foods: Excessive force may dislodge the abutment.
- Poor healing: Issues such as infection or slow healing can lead to instability.
- Incorrect placement: If not properly installed, the healing abutment may not stay secure.
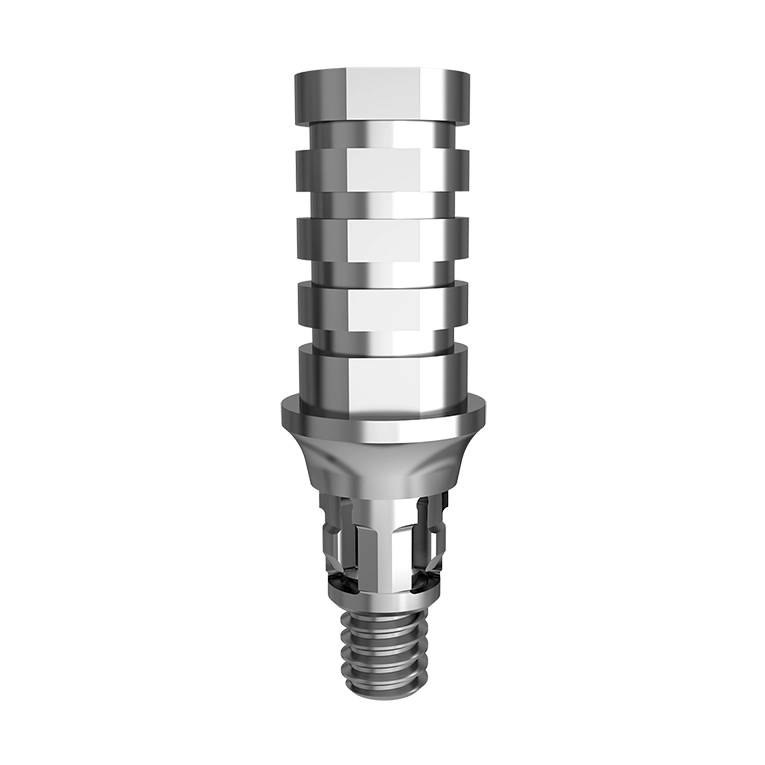
5. What does a healing abutment look like?
Also known as a healing cap, a healing abutment is a temporary device that connects the dental implant with surrounding soft tissues after placement. It is typically made of titanium or other biocompatible materials and often shaped like a cylinder or cone. The surface is specially treated to encourage soft tissue attachment and healing.