In the field of oral restoration, dental implants have brought new hope to many patients troubled by tooth loss or extractions. Often considered the “perfect substitute” for missing teeth, implants help individuals regain both a confident smile and normal oral function. However, peri-implantitis—an inflammatory condition—often silently threatens the health of these implants.
Once peri-implant disease occurs, it signifies that the soft tissues surrounding the implant have become infected and are beginning to deteriorate. Patients may experience pain, swelling, and even difficulties with biting and chewing. Without timely intervention and treatment, the risk of implant failure increases significantly, rendering all previous efforts and expectations futile.
Peri-implantitis is commonly associated with poor oral hygiene, making effective cleaning around the implant essential. In clinical practice, dentists often rely on a specialized tool known as a titanium brush to clean around implants. This tool helps control the progression of inflammation and restores oral health.
So, how can we scientifically and effectively clean peri-implantitis? Let’s explore the proper techniques and methods together.
What Is Peri-Implant Mucositis?
Peri-implant mucositis represents the early stage in the progression of peri-implant diseases—much like gingivitis is the initial phase of periodontal disease. At this stage, the soft tissue surrounding the implant becomes infected, but the underlying bone has not yet been affected.
Compared to the more advanced condition of peri-implantitis, peri-implant mucositis is generally easier to treat. With good oral hygiene habits and regular professional dental cleanings (such as scaling and polishing), patients can effectively prevent the onset of this disease or control it in its early stages, thereby avoiding further deterioration.
However, it’s important to recognize that dental implants have significantly lower resistance to biofilm-induced damage compared to natural teeth. Biofilm is a complex layer of microorganisms, such as bacteria, that forms on the surface of teeth or implants and continuously erodes surrounding oral tissues. Therefore, whether you have implants or natural teeth, preventing peri-implant and periodontal diseases is crucial.
Only through diligent preventive care can we ensure that both artificial and natural teeth remain healthy, stable, and able to serve us well in the long term.
How Common Is Peri-Implantitis?
The actual prevalence of peri-implantitis is not a fixed figure, as it varies depending on the characteristics of the study population and the diagnostic criteria used to define the condition. However, based on multiple research studies, the overall prevalence is estimated to be around 20%.
Certain populations are at a significantly higher risk of developing peri-implantitis. For example, smokers are more vulnerable due to the harmful substances in tobacco, which negatively affect the oral environment and weaken the immune system. Patients with diabetes are also more prone to this condition, as metabolic imbalances can impair tissue healing and reduce resistance to infection. Additionally, individuals who receive inadequate clinical examination may miss early warning signs, allowing the disease to progress undetected.
Particularly noteworthy is the increased risk among patients with long-standing dental implants. As implants remain in the mouth over the years, various biological and mechanical factors accumulate, putting the surrounding tissues under greater stress and increasing the likelihood of peri-implantitis.
What Causes Peri-Implantitis?
Peri-implantitis is often closely linked to poor oral hygiene. When oral health maintenance is inadequate, bacteria can accumulate below the gumline, forming dental plaque and biofilms. These uncontrolled bacteria lead to infections and inflammatory responses in the gums and oral mucosa surrounding the implant.
In addition to inadequate hygiene, several other factors significantly increase the risk of peri-implantitis:
- Smoking: Tobacco use negatively affects blood circulation in the gums, reducing blood flow and impairing tissue health. Smokers are more prone to plaque accumulation, which further raises the risk of infection and inflammation around dental implants.
- Diabetes: Patients with poorly controlled blood sugar levels often have reduced circulation and impaired wound healing. This weakens the body’s ability to fight infection, making the tissues around implants more vulnerable to inflammation.
- Immunosuppression: Individuals with compromised immune systems—such as those with HIV/AIDS or undergoing cancer treatments—are at higher risk, as their bodies are less capable of defending against the pathogens that cause peri-implant and periodontal disease.
- Improper Implant Placement: Incorrect positioning of the implant, or insufficient surrounding bone support, can make the site more susceptible to bacterial invasion and inflammation.
- Excessive Occlusal Force: Overloading the implant through frequent chewing of hard foods or abnormal bite forces can lead to micro-fractures on the implant surface. These micro-damages serve as a breeding ground for bacteria and increase the risk of infection.
- Poorly Fitted Crowns or Restorations: Misaligned or ill-fitting prosthetic components can irritate the peri-implant tissues, causing inflammation and ultimately leading to peri-implantitis.
- Skipping Follow-Up Appointments: Regular follow-ups with a periodontist or dentist are essential after implant surgery. Missing these check-ups can allow minor issues to go unnoticed and develop into serious peri-implant infections.
Common Symptoms of Peri-Implantitis
Peri-implantitis is a potential complication following dental implant surgery that can threaten the long-term stability of the implant and the patient’s overall oral health. Early recognition of symptoms is key to prompt intervention. Below is a detailed overview of the common clinical manifestations:
Gingival Symptoms
- Swelling or Redness: One of the most noticeable signs of peri-implantitis is gingival inflammation around the implant. Healthy gums are typically pink, firm, and closely adhere to the implant or tooth surface. In contrast, inflamed gums appear swollen, engorged, and red or dark red due to vasodilation, increased blood flow, and fluid leakage in response to inflammation.
- Pus Discharge (Suppuration): As the condition progresses, an abscess may form around the implant, leading to the discharge of pus. Patients may notice purulent secretions when brushing, rinsing, or eating. Sometimes, the discharge is accompanied by a foul odor. This occurs when immune cells and tissue undergo necrosis and liquefaction during the body’s battle against infection.
- Pain or Tenderness: Patients may experience pain or tenderness in the gums surrounding the implant, particularly during chewing, brushing, or when the area is touched. The intensity of pain varies—some may only feel slight discomfort, while others suffer severe pain that interferes with daily activities. This is due to the stimulation of nerve endings in the inflamed gingival tissue.
Oral Odor
- Bad Breath (Halitosis): Peri-implantitis is often associated with noticeable bad breath. This is caused by the proliferation of bacteria that decompose food debris and proteins in the oral cavity, producing volatile sulfur compounds and other malodorous substances. The odor may not be apparent to the patient but can be detected by others, potentially affecting the patient’s social interactions and self-esteem.
Changes in Implant Stability
- Implant Mobility: Implant mobility is a more advanced symptom of peri-implantitis. Normally, implants are osseointegrated and firmly anchored in the jawbone. However, inflammation can lead to the destruction of supporting bone, resulting in loss of stability. Patients may feel that the implant shifts when chewing, and in severe cases, the implant may move noticeably with light pressure.
Bone Loss
- Bone Defects or Resorption: Severe peri-implantitis can cause significant bone loss around the implant. Radiographic examinations, such as X-rays or CBCT (Cone Beam Computed Tomography), can reveal reduced bone density, disrupted trabecular structure, and even visible bone defects. Such loss of bone support further compromises implant stability and increases the risk of implant failure.
What Are the Treatment Options for Peri-Implantitis?
Treatment of peri-implantitis primarily includes mechanical debridement and antimicrobial therapy. In more advanced cases, surgical intervention may also be required. Below is a detailed overview of common treatment methods:
Mechanical Debridement
Principle: Specialized instruments are used to remove dental plaque, calculus, and inflamed granulation tissue from the implant surface and surrounding tissues. This directly eliminates sources of irritation, reduces inflammatory mediators, and promotes tissue healing and regeneration.
Common Tools:
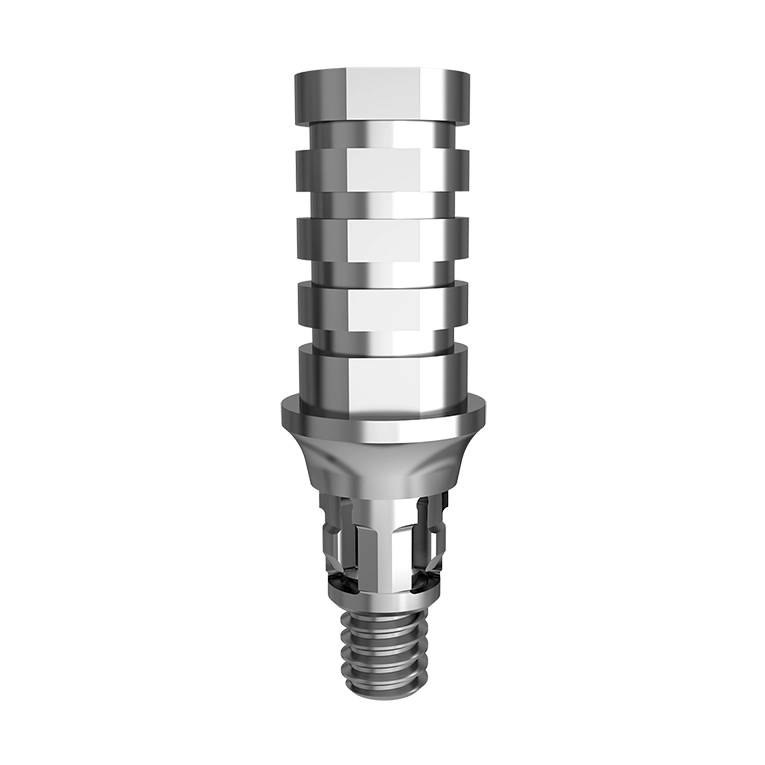
- Titanium Brushes: Operated by periodontists in clinical settings, these brushes effectively remove plaque and calculus from the implant surface and surrounding tissues.
- Ultrasonic Scalers: Use high-frequency vibrations to break and remove calculus deposits.
- Manual Curettes: Allow for more precise cleaning of the implant surface and infected periodontal pockets.
- Air Abrasion (Sandblasting): Offers good cleaning efficiency. However, the abrasive material affects both cleaning results and surface roughness. For example, large-particle sodium bicarbonate is effective but significantly increases surface roughness.
Antimicrobial Therapy
Antibacterial Mouthwash:
- Chlorhexidine Gluconate: A commonly used antimicrobial mouth rinse for peri-implantitis. A 0.12% solution can effectively reduce the risk of peri-implant inflammation by inhibiting bacterial colonization. However, a 2% concentration may irreversibly inhibit cell migration and significantly reduce the viability of fibroblasts, myoblasts, and osteoblasts in vitro—warranting further research on safety and efficacy.
- Other Mouthwashes: Compound borax rinse, combination chlorhexidine formulations, etc., may be used under a dentist’s guidance.
Topical Gels:
Minocycline Hydrochloride Ointment: Can be applied locally or injected into the affected site to help eliminate bacteria and control infection.
Oral Medications:
For more severe infections, systemic antibiotics may be prescribed, such as Metronidazole, Tinidazole, Amoxicillin, or Roxithromycin. These should only be taken under professional medical supervision.
Surgical Treatment
Indications: When peri-implantitis is severe and non-surgical treatments have controlled the infection but alveolar bone defects remain, surgical procedures may be necessary.
Common Surgical Techniques:
- Osteoplasty (Bone Recontouring): Reshapes damaged alveolar bone to support healing.
- Bone Grafting: Fills areas of bone loss to stimulate bone regeneration.
- Flap Surgery with Debridement: Involves lifting the gum flap to remove infected tissue and applying biomaterials to preserve bone density and promote cell proliferation in the defect area.
- Guided Tissue Regeneration (GTR): A bio-membrane is placed over the bone defect to prevent soft tissue invasion, providing a space for new bone formation.
- Implant Removal: In cases of extensive bone destruction and implant mobility, surgical removal of the implant may be necessary.
How to Prevent Peri-Implantitis
Preventing peri-implantitis requires comprehensive care, including daily oral hygiene, healthy lifestyle adjustments, and regular professional follow-ups. Here’s a detailed guide:
Daily Oral Hygiene
Proper Brushing Techniques
- Choose the Right Toothbrush: Use a soft-bristled, small-headed toothbrush to effectively clean around the implant without irritating the gums. Specialized brushes designed for dental implants offer softer bristles and ergonomic brush heads that fit the oral structure better.
- Master the Brushing Method: Use the Bass technique — hold the toothbrush at a 45° angle toward the root, positioning the bristles partly in the gum sulcus and partly on the gum line. Gently vibrate in short horizontal motions (about 1 mm) 10 times per section, covering 2–3 teeth at a time, and overlap the brushing area as you move. Brush at least twice a day for no less than 3 minutes each time.
Use of Dental Floss, Interdental Brushes, and Oral Irrigators
- Dental Floss: Implant sites are prone to food debris retention between teeth. Gently slide the floss into the gap and move it up and down to clean the interproximal surfaces.
- Interdental Brushes: Ideal for larger gaps or specific implant structures. Choose the appropriate size and gently move the brush back and forth.
- Oral Irrigators: Use high-pressure water jets to remove debris and bacteria from hard-to-reach areas. Use once or twice daily for optimal cleanliness.
Clean the Implant Crown or Prosthetic Structure
Use a soft-bristled toothbrush to gently clean the surface of the implant crown or restoration. Avoid hard or sharp tools to prevent scratching the implant surface.
Lifestyle Adjustments
Quit Smoking
Smoking reduces blood flow in the gums and weakens immune defenses, making implants more vulnerable to infection. Studies show that smokers are 2–3 times more likely to develop peri-implantitis. Quitting smoking is essential for maintaining implant health.
Control Blood Sugar
People with diabetes are at higher risk due to impaired circulation and slower healing. Strictly follow medical advice to keep blood sugar levels within a normal range through regular monitoring and medication.
Avoid Excessive Chewing Forces
Avoid chewing hard foods (e.g., nuts, crab shells) with implants. Excessive pressure can damage the implant or restoration and increase the risk of inflammation. Choose food with moderate texture and chew evenly on both sides.
Regular Checkups and Maintenance
Routine Dental Checkups
Follow your dentist’s schedule for follow-ups: typically at 1, 3, and 6 months after implant placement, then at least once or twice a year. Dentists will assess the health of surrounding tissues using tools like X-rays and probing to detect early signs of complications.
Professional Cleaning
In addition to home care, regular professional cleaning is essential. Dental professionals use specialized tools, such as ultrasonic scalers and curettes, to thoroughly remove plaque and tartar around implants, helping prevent peri-implantitis.
Can peri-implantitis go away on its own?
Peri-Implantitis Generally Cannot Heal on Its Own, but Early-Stage Cases May Be Clinically Curable with Simple Treatment
Peri-implantitis is an inflammatory disease affecting the soft and hard tissues surrounding a dental implant. It is primarily caused by poor oral hygiene, which leads to the accumulation of plaque and calculus on the implant surface. This buildup triggers an immune response, resulting in inflammation of the surrounding soft tissue and gradual resorption of the alveolar bone.
As the condition progresses, the bond between the implant and surrounding tissues becomes compromised. This damage is typically progressive and ongoing, and the body has limited ability to naturally repair the inflammation and tissue destruction.
Without timely intervention, the inflammation may worsen, leading to further bone loss and separation at the implant–bone interface. Eventually, this can cause implant loosening or even complete implant failure. Clinically, once peri-implantitis sets in, the body’s immune system alone is usually insufficient to restore health. This is because a dental implant is a foreign object, and the inflammatory response around an implant differs from that of natural teeth. As a result, the body’s repair capabilities are relatively limited.
However, in the early stages of peri-implantitis—when the inflammation is still confined to the soft tissues (mucositis)—simple treatment measures can often achieve clinical resolution.