In the field of oral implant restoration, dental implants have brought renewed hope to many patients suffering from tooth extraction or loss, enabling them to regain a healthy smile and normal chewing function. However, peri-implantitis—an inflammatory disease—lurks like a hidden “destroyer,” silently threatening the health and stability of dental implants.
Peri-implant diseases target the soft tissues surrounding the implant. Once these tissues become infected, a destructive process is set in motion. Patients often endure pain and swelling, and everyday functions such as biting and chewing become increasingly difficult. Without timely and effective treatment, the risk of implant failure increases significantly, potentially rendering all the effort and anticipation invested in the implant procedure meaningless.
So, how should we respond to the challenging problem of peri-implantitis? Poor oral hygiene is considered one of the primary culprits behind this condition. A combination of deep cleaning and antimicrobial therapy is commonly used as a treatment approach. However, in more severe cases, the difficult decision to remove and replace the implant may be unavoidable. Next, let’s take a closer look at effective strategies for managing peri-implantitis.
What is Peri-Implant Mucositis?
Peri-implant mucositis is the early stage of peri-implant diseases and shares many similarities with gingivitis—the initial phase of gum disease in natural teeth. At this stage, inflammation occurs in the soft tissue surrounding the dental implant, but the deeper bone structures have not yet been affected.
Compared to the more advanced condition of peri-implantitis, peri-implant mucositis is significantly easier to treat. With proper oral hygiene practices—such as brushing thoroughly every day, using dental floss to clean between teeth, and regularly visiting a dental professional for cleanings—this issue can be effectively prevented, and even reversed in its early stages.
However, it’s important to recognize that dental implants are inherently less resistant than natural teeth to the buildup of biofilm—a complex bacterial structure that forms on the surface of teeth and implants. If not removed in a timely manner, biofilm can lead to inflammation. Therefore, whether you have dental implants or natural teeth, preventing both peri-implant and periodontal diseases is essential. Only through consistent and effective preventive care can you ensure the long-term health and stability of both your artificial and natural teeth.
What Are the Causes of Peri-Implantitis?
1. Poor Oral Hygiene:
Plaque accumulation on the implant surface is the leading cause of peri-implantitis. The harmful bacteria in plaque can infect the surrounding tissues of the implant, trigger inflammation, and even lead to alveolar bone loss.
2. Local Contributing Factors:
- Improper Prosthetic Design: A poorly designed restoration can make plaque control difficult, increasing the risk of infection.
- Excessive Load on the Implant: If the implant is subjected to excessive biting or chewing forces, it can accelerate bone loss and damage surrounding tissues.
- Rough Implant Surface: Implants with rough surfaces are more prone to plaque buildup, increasing the likelihood of infection.
- History of Periodontitis: If other natural teeth are affected by periodontitis, the bacteria can spread to the implant site, causing peri-implantitis.
3. Harmful Habits:
- Smoking: Smoking is a significant risk factor for peri-implantitis. Harmful substances in tobacco can impair local blood circulation, slow tissue healing, and suppress immune function.
- Excessive Alcohol Consumption: Heavy drinking may also increase the risk of developing peri-implantitis.
4. Systemic Conditions:
- Diabetes: Uncontrolled diabetes reduces blood flow, impairing the body’s ability to heal from infections or injuries and raising the risk of peri-implantitis.
- Osteoporosis: This condition may hinder the integration of the implant with the surrounding bone, increasing vulnerability to infection.
- Immunosuppression: Patients with compromised immune systems (e.g., those with HIV/AIDS or undergoing cancer treatment) are more susceptible to infections, including peri-implantitis.
5. Improper Implant Placement or Lack of Bone Support:
If the implant is not placed correctly or there’s insufficient supporting bone, the risk of bacterial infection around the implant rises.
6. Overloading the Implant:
Applying excessive force to the implant—such as biting or chewing hard objects—can accelerate wear and damage. This creates niches for bacteria and promotes inflammation.
7. Poorly Fitting Crowns or Restorations:
If crowns or other prosthetic components do not fit properly, they can irritate the surrounding tissues and lead to inflammation and peri-implantitis.
8. Missed Follow-Up Appointments:
Regular follow-up visits after implant placement are crucial for identifying and addressing potential issues early. Skipping these appointments can allow minor problems to escalate into serious complications.
Detailed Symptoms of Peri-Implantitis
1. Gum-Related Symptoms
- Swelling or Redness of the Gums:
When peri-implantitis occurs, inflammation stimulates the gum tissue surrounding the implant, causing it to become congested and swollen. Unlike healthy gums—which are pink and firm—inflamed gums appear red and puffy. The degree of swelling may worsen over time. In the early stages, swelling might be localized and mild, but as the condition progresses, it can spread to nearby gum areas. - Pain or Tenderness in the Gums:
Inflammation damages local tissues and irritates nerve endings, which leads to pain or tenderness around the implant site. Patients may feel discomfort when eating, brushing, or touching the affected area. Pain intensity varies—mild cases may only cause slight discomfort, while severe cases can cause significant pain that disrupts daily activities and eating. - Pus Discharge (Suppuration):
If the inflammation progresses to a purulent infection, pus may begin to discharge around the implant. Pus is a mixture of dead tissue, white blood cells, and bacteria formed during the immune response. It may ooze from the gum margin or the gap between the implant and the gums and is often accompanied by a foul odor, indicating a more advanced infection.
2. Bad Breath (Halitosis):
Peri-implantitis leads to localized infection, allowing bacteria to accumulate around the implant. These bacteria release malodorous substances—such as hydrogen sulfide—during their metabolic process, causing noticeable bad breath. This odor is usually persistent, and patients may notice it themselves. It can also be detected by others during close contact, affecting social interactions and psychological well-being.
3. Implant Mobility:
Peri-implantitis can result in bone loss and deterioration around the implant. The alveolar bone supports the implant, and once it’s compromised, the implant begins to lose stability. Early-stage mobility might not be noticeable to the patient, but dentists can detect it with professional tools. As the condition worsens, the mobility becomes more evident—patients may feel the implant shifting or moving, which can interfere with chewing function.
4. Severe Tissue Damage and Bone Loss:
- Tissue Damage:
If peri-implantitis is left untreated, inflammation may continue to spread and worsen, causing extensive damage to the tissues surrounding the implant. Beyond the gums and bone, nearby soft tissues—like the oral mucosa—may also become involved, leading to symptoms such as redness, swelling, and ulceration. This can significantly affect oral health and function. - Bone Loss:
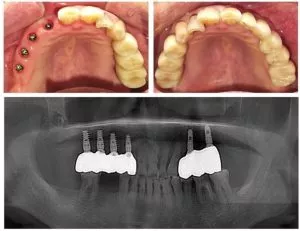
One of the most serious consequences of peri-implantitis is bone resorption. Inflammation activates osteoclasts (bone-resorbing cells), which gradually destroy the alveolar bone around the implant. X-rays or other imaging techniques can reveal reduced bone height and density. Bone loss compromises implant stability, increases the risk of implant failure, and may even lead to changes in facial appearance—such as facial sagging—which negatively impacts both oral function and aesthetics.
Detailed Stages of Peri-Implantitis
1. Initial Inflammation (Early Stage)
Gum Symptoms: This is the onset phase of peri-implantitis, where the gums around the dental implant begin to show signs of redness and swelling. Similar to gingivitis, the normally pink, firm gums become inflamed and swollen. At this stage, inflammation is relatively localized and mainly affects the gingival tissues.
Cause: The primary trigger is typically the accumulation of bacteria on the surface of the implant. Since the oral cavity is rich in bacteria, poor daily oral hygiene can lead to the formation of a bacterial biofilm on the implant surface, which then triggers an inflammatory response.
2. Peri-Implantitis with Bone Loss (Progressive Stage)
Inflammation Progression: As the condition worsens, the inflammation around the implant deepens and spreads beyond the gum tissue, beginning to affect the supporting alveolar bone.
Bone Loss: Inflammatory stimuli activate osteoclasts, leading to resorption and destruction of the surrounding alveolar bone. This bone loss is similar to what occurs in periodontitis but may progress more rapidly and severely around implants due to structural differences from natural teeth.
Gum Symptoms: The gums may become more swollen and painful. Patients will feel clear discomfort around the implant, and activities like eating or brushing may worsen the pain.
3. Advanced Peri-Implantitis (Severe Stage)
Worsening Inflammation and Bone Loss: At this point, inflammation and bone resorption become significantly worse. Ongoing inflammation continually damages the surrounding tissues, and a large amount of alveolar bone may be lost, greatly compromising the support around the implant.
Implant Mobility: Due to severe bone destruction, the implant loses sufficient bony support and becomes noticeably loose—similar to how a tree becomes unstable when the surrounding soil is heavily eroded.
Signs of Infection: There may be clear signs of infection, such as pus oozing from the area around the implant. Pus is a mix of dead tissue, white blood cells, and bacteria, indicating a serious infection.
4. Failure Stage
Implant Outcome: If peri-implantitis is left untreated, the condition can continue to worsen and ultimately result in implant failure. At this point, the implant can no longer function properly and must be removed.
Follow-Up Treatment: After removal, severe bone loss may require regenerative procedures or bone grafting to rebuild the alveolar ridge before considering another implant. This increases the complexity, cost, and duration of treatment.
Diagnosis and Treatment Essentials
Diagnosis Methods: Periodontists can use advanced tools like X-rays to assess the progression of peri-implantitis. X-ray images help visualize bone height, density, and the relationship between the implant and surrounding tissues, allowing for accurate assessment of disease severity.
Treatment Keys: Early detection and proper intervention can prevent serious damage and save the implant. Successful treatment requires a periodontist’s expertise, who will create a personalized treatment plan based on the severity of the condition. This may include oral hygiene guidance, mechanical debridement, and medication.
Can Peri-Implantitis Be Reversed?
While peri-implantitis can be treated and its progression can be halted with proper intervention, it is not always fully reversible. The success of treatment largely depends on the severity of the condition and how early the treatment begins.
In the early stages of peri-implantitis, the damage to surrounding tissues is relatively mild. At this point, the condition can often be reversed through procedures such as scaling and root planing (a deep cleaning method for teeth and implant surfaces), along with the use of antibacterial mouth rinses or gels. These treatments help effectively remove plaque and calculus from the implant surface, reduce bacterial load, and alleviate the inflammatory response.
However, if the condition has progressed to a more advanced stage, non-surgical treatments alone may not be sufficient to fully reverse the damage. In such cases, further measures may be necessary, such as surgical removal of infected tissue to thoroughly eliminate the source of infection, or bone grafting to restore bone loss caused by inflammation. While these treatments are more complex, they are essential for controlling the disease and preventing implant failure when necessary.
Treatment Methods for Peri-Implantitis
The treatment of peri-implantitis is a comprehensive and systematic process aimed at eliminating the underlying causes, controlling infection, and restoring the health of the tissues surrounding the implant. Below is a detailed overview of the treatment methods:
1. Mechanical Debridement
Mechanical debridement is a fundamental part of peri-implantitis treatment. It involves physically removing pathogenic factors from the implant surface and surrounding tissues to create favorable conditions for further treatment.
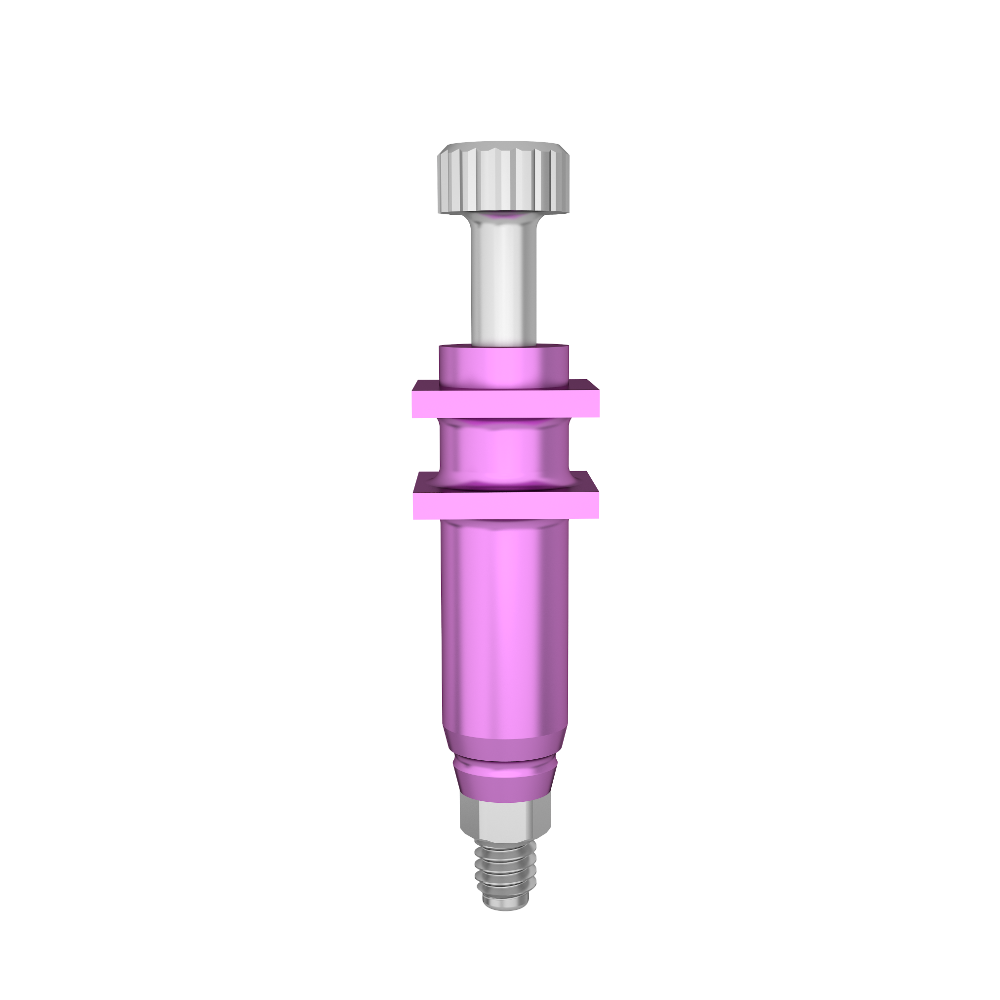
Specialized Instruments
- Titanium Brushes: Titanium brushes are specifically designed for cleaning implant surfaces. Due to the unique microstructure of implants, plaque and calculus tend to adhere tightly, making it difficult for regular tools to remove them effectively. The bristles and design of titanium brushes conform to the implant surface, effectively eliminating plaque and calculus while reducing bacterial load.
Clinical Procedure
Mechanical debridement should be performed in a professional dental setting by a periodontist. The dentist will select appropriate instruments and techniques based on the severity of the condition and the type of implant. During the procedure, the dentist will operate carefully and gently to avoid unnecessary damage to the implant or surrounding tissues.
2. Antimicrobial Therapy
The goal of antimicrobial therapy is to eliminate bacteria, control infection, and prevent further inflammation. Depending on the severity of the condition and the patient’s situation, various methods may be used.
Antibacterial Mouthwash
- Chlorhexidine Gluconate: A commonly used antibacterial mouthwash for treating peri-implantitis, chlorhexidine has broad-spectrum antimicrobial effects that inhibit the growth of various oral bacteria. Patients are advised to rinse several times a day using a prescribed concentration for a specific duration to reduce the bacterial load and alleviate inflammation.
- Cetylpyridinium Chloride (CPC) Mouthwash: CPC also has antibacterial and anti-inflammatory effects. It alters the permeability of bacterial cell membranes, causing intracellular contents to leak out, which helps kill the bacteria.
Topical Antibacterial Gels
Dentists may apply antibacterial gels directly around the implant. These gels contain antimicrobial agents that act locally on the infected area, increasing the concentration of the medication and enhancing antibacterial effectiveness. For example, topical gels containing minocycline can effectively suppress bacterial growth at the site of inflammation and promote healing.
Systemic Antibiotics
For more severe cases or widespread infections, oral or intravenous antibiotics may be prescribed. Commonly used antibiotics include amoxicillin and metronidazole. The dentist will determine the appropriate antibiotics based on bacterial culture and sensitivity tests to ensure effective treatment.
3. Surgical Treatment
If peri-implantitis has progressed and non-surgical methods fail to produce satisfactory results, surgical intervention becomes necessary to thoroughly remove infected tissues and repair damaged alveolar bone.
Flap Surgery
- Procedure: The dentist makes an incision in the gum around the implant and lifts the tissue to expose the implant surface and surrounding bone. This allows for better visualization and complete removal of plaque, calculus, and infected granulation tissue.
- Postoperative Care: After flap surgery, the gums are sutured, and healing-promoting agents or materials may be placed. Patients must follow postoperative oral care instructions to maintain hygiene and prevent infection.
Guided Bone Regeneration (GBR)
- Indications: If the peri-implantitis has led to significant bone loss and compromised implant stability, GBR may be necessary.
- Surgical Principle: After debridement and infection control, bone graft materials such as synthetic bone powder or autologous bone are placed in the defect area. A bio-membrane is then used to cover the site. This membrane prevents soft tissue from growing into the bone defect area, creating a protected space that promotes bone regeneration and healing.
Methods for Preventing Peri-Implantitis
Peri-implantitis can severely affect the longevity of dental implants and overall oral health. Preventing its occurrence is essential and should be addressed from multiple stages: pre-operative, intra-operative, and post-operative.
Pre-Operative
Comprehensive Oral Examination and Treatment
- Examinations: Before dental implant surgery, a thorough oral examination is necessary. This includes assessing the teeth, gums, alveolar bone, and general health condition. Imaging techniques such as panoramic X-rays and CT scans help evaluate the shape, density, and height of the alveolar bone, as well as its relationship with nearby anatomical structures (e.g., mandibular canal, maxillary sinus) to ensure sufficient bone volume for implant placement.
- Treatment of Diseases: Any existing oral diseases such as cavities or periodontitis must be treated beforehand. For example, untreated periodontitis—a major risk factor for peri-implantitis—can lead to a bacterial and inflammatory environment around the implant. Therefore, dental plaque and calculus should be thoroughly removed, and inflammation should be controlled before proceeding with implantation.
Systemic Health Evaluation and Management
- Assessment: General health also impacts implant success. Conditions like diabetes, cardiovascular disease, or immune disorders may raise the risk of peri-implantitis. For instance, poorly controlled diabetes compromises immunity and healing, increasing susceptibility to infection around the implant.
- Management: Patients with systemic diseases should have their conditions stabilized before implant surgery. Diabetics should maintain proper blood glucose levels, and those with heart conditions should follow medical guidance to minimize inflammation risk.
Intra-Operative
Strict Aseptic Technique
- Sterile Protocols: Implant surgery must be carried out in a sterile environment. The operating room and instruments should be thoroughly disinfected and sterilized. Surgeons must wear sterile gloves, masks, and caps, and strictly follow aseptic procedures to avoid contamination.
- Infection Prevention: Any bacterial contamination can cause peri-implantitis. If instruments aren’t fully sterilized or the surgeon’s hand hygiene is inadequate, bacteria may enter the surgical site and cause infection.
Accurate Implant Placement
- Positioning and Angulation: The implant must be placed at the correct position and angle according to the preoperative plan. Improper placement can impair the bond between the implant and bone or cause excessive pressure on surrounding soft tissue, increasing inflammation risk.
- Tissue Protection: During the procedure, care must be taken to avoid unnecessary trauma. For example, when raising a flap, handle tissues gently to avoid gum damage; when drilling, control speed and force to prevent bone injury.
Post-Operative
Oral Hygiene Maintenance
- Brushing Technique: Patients should adopt proper brushing techniques, such as the Bass method, brushing at least twice a day for three minutes each time. A soft-bristle toothbrush is recommended to avoid damaging the gums around the implant.
- Additional Cleaning Tools: Besides brushing, tools like dental floss, interdental brushes, and oral irrigators should be used. Floss cleans between teeth and around the implant, while interdental brushes help in areas with larger gaps. Oral irrigators use water pressure to flush out food debris and bacteria, ensuring oral cleanliness.
Regular Check-Ups and Maintenance
- Check-Up Schedule: Patients should follow their dentist’s recommended schedule, typically every three months during the first year, then every six to twelve months.
- Check-Up Content: Dentists will assess implant stability, gum health, and bone levels. If early signs of inflammation—such as gum redness or bleeding—are detected, timely intervention like scaling or curettage can prevent progression.
Lifestyle Adjustments
- Dietary Habits: Avoid hard foods (e.g., nuts, crab shells) that may exert excessive force on the implant, leading to loosening or bone resorption. Reduce smoking and alcohol consumption, as smoking impairs blood circulation and immune response, while alcohol may interfere with medication and tissue healing.
- Injury Prevention: Protect the implant from trauma. During intense physical activities, consider wearing a mouthguard to prevent damage from impacts.
Home Treatment and Precautions for Peri-Implantitis
If peri-implantitis is in its early or mild stages, proper at-home oral care can help control the condition and slow its progression. However, it’s important to understand that home treatment cannot replace professional medical intervention. If the condition worsens or persists, seek professional care promptly. Below are specific methods and key points for home treatment:
1. Oral Hygiene Measures
Proper Brushing Techniques
- Frequency and Method: Brush at least twice daily using the modified Bass technique. Hold the toothbrush at a 45° angle to the tooth axis, pointing toward the gum line. Allow part of the bristles to enter the gingival sulcus and part to rest on the gum line. Gently vibrate the brush back and forth in short horizontal strokes (about 1 mm) 10 times for each section of 2–3 teeth. When moving to the next section, overlap slightly to ensure thorough cleaning. Pay special attention to the area where the implant meets the gum tissue. Use gentle movements to avoid gum damage.
- Toothbrush Selection: Use a soft-bristled, small-headed toothbrush to better reach the narrow spaces around the implant and minimize irritation to the gums and implant area.
Using Dental Floss
- How to Use: Floss daily to clean the spaces between the implant and adjacent teeth. Gently insert the floss, curve it into a C-shape around the tooth surface, and slide it up and down to remove debris and plaque. Be extra cautious around implants to avoid injuring surrounding tissues.
- Floss Type: Choose either regular floss or floss specifically designed for implants, which tends to be softer and better suited to the implant structure.
Additional Cleaning Tools
- Interdental Brushes: If gaps around the implant are wide, use an interdental brush. Choose a size that matches the gap and gently move it back and forth to remove plaque from the implant surface.
- Oral Irrigators (Water Flossers): These devices use a high-pressure stream of water to rinse food particles and bacteria from the tooth surface, gaps, and around the implant. Direct the nozzle around the implant and clean in an inside-to-outside, top-to-bottom sequence. Use once or twice daily.
2. Use of Antibacterial Mouthwash
Choosing the Right Mouthwash
- Opt for mouthwashes containing antibacterial ingredients like chlorhexidine or cetylpyridinium chloride. For example, chlorhexidine gluconate has broad-spectrum antibacterial properties and effectively reduces plaque and bacterial growth in the mouth.
How to Use
- Follow the product instructions. Rinse once or twice daily for 1–2 minutes each time, then spit out. Avoid rinsing with water immediately after to ensure maximum effectiveness. Note that chlorhexidine mouthwash should not be used long-term, as it may cause tooth staining and alter taste perception. It is generally recommended not to exceed two weeks of continuous use.
3. Lifestyle Adjustments
Dietary Considerations
- Avoid Irritants: Limit consumption of spicy, acidic, extremely hot or cold foods, as they can irritate the gum tissue around the implant and worsen inflammation. Foods like chili, lemon, and ice cream should be minimized.
- Control Food Hardness: Avoid chewing hard foods like nuts, crab shells, or sugarcane. Excessive biting force may loosen the implant or damage surrounding bone tissue.
Quit Smoking and Limit Alcohol
- Quit Smoking: Smoking impairs blood circulation in the mouth, reduces immune response, and increases the risk of peri-implantitis. Studies show that smokers have a significantly higher rate of implant inflammation compared to non-smokers. Quitting smoking is essential for implant health.
- Limit Alcohol: Excessive drinking may weaken the immune system and hinder healing of tissues around the implant. It’s best to limit or avoid alcohol.
4. Regular Check-Ups and Professional Maintenance
Routine Dental Visits
- Even with good home care, regular visits to a periodontist are crucial for professional cleaning and assessment. Typically, post-surgery reviews should be scheduled every three months in the first year, then every six months to a year afterward.
Professional Cleaning
- Dentists use specialized tools, such as titanium brushes, to deeply clean the implant and remove plaque and tartar, especially from threads and hidden areas. They will also assess the implant’s stability, gum health, and bone levels, identifying and addressing any potential issues early.
Conclusion
Peri-implantitis remains one of the major challenges in the field of dental implants. If not properly managed, it can lead to implant failure, severely affecting the patient’s oral health and overall quality of life. However, by combining professional treatment with diligent at-home care, we can effectively combat this condition.
From a clinical standpoint, mechanical debridement is the foundational and essential step in treatment. Titanium brushes, specifically designed for cleaning implants, play an irreplaceable role. Their unique materials and bristle design allow for precise contact with the implant surface, effectively removing plaque and calculus, and preparing the area for further treatment. In addition, antimicrobial therapy is crucial—whether through medicated mouth rinses, topical gels, or systemic antibiotics when necessary, these interventions help eliminate bacteria, control infection, and prevent further inflammation. For more severe cases, surgical procedures such as flap surgery or guided bone regeneration may be required to remove diseased tissue and restore lost bone, thereby improving the implant environment at its core.
At the same time, patients have an equally vital role in home care. Maintaining good oral hygiene is central to both preventing and managing peri-implantitis. Brushing twice daily with proper technique and carefully cleaning around the implant, along with using interdental brushes, dental floss, and water flossers, ensures thorough removal of food debris and bacteria and limits plaque accumulation. The controlled use of antimicrobial mouthwash can further eliminate hidden bacteria and reduce the risk of infection. Moreover, adopting healthier lifestyle habits—such as avoiding hard or spicy foods and quitting smoking or limiting alcohol intake—helps protect gum tissue and supports healing around the implant.
Regular follow-ups and professional maintenance with a periodontist should not be overlooked. With their expertise, dentists can detect early signs of peri-implantitis and provide timely intervention. Routine deep cleanings and comprehensive check-ups ensure the long-term health and stability of the dental implant.
In summary, the successful treatment of peri-implantitis requires close cooperation between dental professionals and patients. While clinicians develop personalized treatment plans based on their expertise and experience, patients must remain committed to strict home care routines and follow medical advice. Together, this partnership not only enhances the success rate of dental implants but also extends their lifespan—helping patients regain a healthy, confident smile.